On Research Metabolism and Ketones with Dr. Latt Mansor – Ep. 183
Sep 30, 2022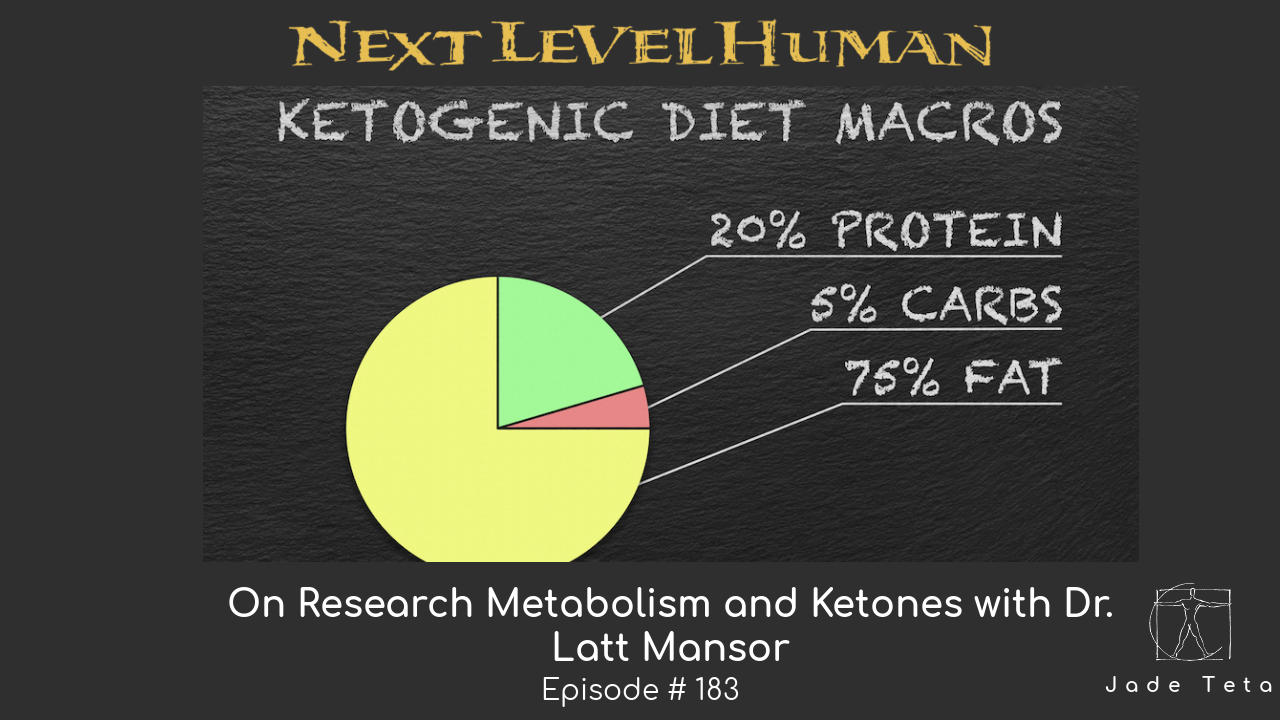
In this episode of Next Level Human Podcast, Dr. Jade connects with Dr. Latt Mansor. Dr. Mansor is the Research Lead at HVMN and has a background in metabolism and physiology. Today, he talks about how ketones impact almost everything in our bodies and how they can improve performance, body functions, and overall energy.
Dr. Mansor also explains that inflammation in the body and even chronic diseases such as diabetes and hypertension can all be caused – or at least influenced – by our diet. One way to start optimizing our daily diet is by looking at insulin levels: high levels of insulin tend to be responsible for these issues and are also connected with our daily carbohydrate intake.
In addition, Dr. Mansor also dives deep into ‘exogenous ketones’. Exogenous ketones are ketones we can take from outside sources (like a supplement) but he explains that if an individual is already following a ketogenic diet to lose weight (meaning ketones are already being made by the body) there is no need to benefit from this alternative. Tune in!
Check out the Next Level Human sponsors!
- Go to drinklmnt.com/NEXTLEVEL to claim your free LMNT Sample Pack with any purchase.
- Visit https://paleovalley.com/nextlevel to learn more about the gut-friendly 100% grass-fed beef sticks and save 15%!
Connect with Dr. Latt Mansor
Instagram: @lattmansor
Instagram: @hvmn
Website: hvmn.com
Connect with Dr. Jade Teta
Website: www.jadeteta.com
Instagram: @jadeteta
TRANSCRIPTION:
Podcast Intro: [00:14] welcome to the Next Level Human Podcast. As a human, you have a job to do. In fact, you have four jobs; to earn and manage money, to attain and maintain health and fitness, to build and sustain personal relationships, to find meaning and make a difference. None of these jobs are taught in school and that is what this podcast is designed to do. To educate us all on living our most fulfilled lives through the mastery of these four jobs. I'm your host, Dr. Jade Teta and I believe we are here living this life for three reasons and three reasons only; to learn, to teach and to love. In this podcast, I will be learning, teaching, and loving right along with you. I'm grateful to have your company; here is to our next level.
All right, everybody. Welcome to today's show. So I have a guest today who I'm meeting for the first time. Matter of fact, we just met about three minutes ago as we connected on to the platform here. This is Dr. Latt Mansor Ph. D. By the way, Latt is suffering from a little bit of a cold. So, he let me know that as we popped on, so he may have a little bit of a cough. But one of the reasons I got excited, we got hooked up by Chase Chewning, who's a mutual friend of ours, who oftentimes suggest people for this podcast and one of the reasons I got excited about talking to you because when I looked at your, you know, sort of areas of expertise, I was just like, oh, this is my man like he's, he's got deep understanding in metabolism in chronic disease. In psychology, he's a, he's an expert in ketones and exogenous ketones, the list goes on and on and on. But one of the things that I wanted to do with Latt is just discuss deep dive metabolism. Here we have a PhD, who has studied this stuff, who deep dives into this stuff all the time, and is looking at it at a very high level in the research, and so why not discuss that. So Latt thank you so much for being here for taking time out to talk to the next level human podcast, just to let you know, most of the people on this podcast are pretty advanced fitness enthusiast, a lot of them are clinicians. So it's going to be a really fun time for them to get, you know, sort of your expertise and have us have this discussion. But to start out, why don't you just give us sort of a brief into your background, how you got into this work, what your interests are, and then we can go from there?
Latt 3:11
Sure, I thank you very much Jade for having me on your podcast. I'm looking forward to this as well. Because prior to this, I did look at your website, and I did see your area of expertise in Tableau ism, as well as your hands on experience in training people. Because what I do is what we discover in lab, what we investigate from a mechanism point of view, but what you do is essentially putting that knowledge and information in application and actually see it working on different, you know, individuals. So it's definitely very excited to hear your opinion on certain things and your experience in applying these knowledges. So in terms of background, I am currently the research lead of HVMN health via modern nutrition. I am in charge of all the r&d research collaborations with universities institutions. I'm also the principal investigator of our $6 million DoD grant contract to look at exogenous ketones in humans, looking at physical and cognitive performance, especially in hypoxia, which means low oxygen environment. And that brings me to my PhD, which was essentially my research doing cardiac metabolism in type two diabetic heart in hypoxia. So I use hypoxia as a subset of ischemia, which is, you know, lack of blood flow or occlusion of, of the artery that leads to usually myocardial infarction, which is heart attack. So that's my PhD and from University of Oxford and physiology, anatomy and genetics, and prior to that I was working for a pharmaceutical company in clinical operations Space in New Jersey. That was right after my master's I did my masters in biotechnology, from Columbia Union. Firstly, in New York, that was my first time in the US. And my undergrad was from University of Nottingham, in the UK, also in biotechnology. And originally I'm from Malaysia born and bred, I didn't leave the country until I was 20. So that was my first time abroad, went to UK went to us back to UK for my PhD, well, I actually went to Germany first worked for a year for the pharmaceutical company, and then went back to school and the UK, just because the PhD in UK takes three years, whereas in the US, it takes longer than that. So I decided to go back there.
Jade 5:33
Well Latt we're really, really lucky to have someone of your caliber on the show. One of the things I love about the PhD researchers, the ones that are on the ground doing the research is that we don't oftentimes get a chance to talk to them. And one of the first things I want to ask you about is this idea, because one of the things that happens is when we're dealing with someone like Latt, and other PhDs who are on the ground, sort of doing the research, and then that research goes into the journals, and those journals come out to clinicians and the public, and especially the media, this stuff has to get translated from the researchers who are doing it into the people who are using it on the ground. And oftentimes a lot gets lost in that translation. And so one of the things that I want to ask you just right off the bat, and maybe you can give us some pointers and tidbits about this is when you as a researcher, and when you look at this stuff, how would you? Do you think it's a problem, this translation problem, the fact that people are getting things wrong? If you do think it's a problem? How, how would you suggest that clinicians like myself and the lay public began to look at research. And to kind of get you started on this, I'll just give you a couple of my pet peeves that you may or may not agree with, which is just fine. I love when we kind of get into this one of my pet peeves is the fact that, you know, individuals who are not used to or understand the science will often allow their bias what they what works for them, or what they mostly read, to determine their, you know, opinions. And then those opinions turned into identities. And then those identities become, you know, a situation where we're battling each other. And this has always sort of bothered me, and I wonder how you, as a researcher sees this and what insights and sort of tips you can give us around this idea of what happens from the research to the translation to the clinics and everyone else?
Latt 7:28
Yeah, that's an amazing question. And I'm glad you brought that up as well. Because I think during my master's period, when I was doing my Masters, I think that was when I realized there is a disparity, there's a disconnect between academia, and industry and application and to the general public. And that was, when I realized what I like to do, I want to find a job where I can bridge essentially the knowledge from academia to the general public, because I don't want to just stay in the lab all my life and just, you know, doing all these cool science, you know, discovering cool stuff, and coming up with the best, you know, mechanism of action of certain drugs and get Nobel Prize. Like, while that is super cool, I feel like those, like you said, there's a lot that is being lost in translation. And right now I am, you know, I would say, so far, I'm very, very happy where I am, because I get to do science, I get to still conduct all these studies, and also talk with all these researchers, but at the same time, being on podcast like this, to be able to convey that knowledge and information to the general public. So in terms of tips, what I would say, is always go into a research or I mean, always read a research with an open mind, right? As you said, do not let your biasness cloud your judgment, or let your biasness cloud the way you read the research, and a lot of these research, especially when it comes to metabolism. There's a lot of nuance that's involved. What's the difference in gender? What's the difference in age, what's the difference and protocol. Now for our area, for example, exogenous ketones is still very, very new. So when it's so new, there are multiple types of protocols that people employ in order to test whether these exogenous ketones work, whether it works in acute setting and pre workout setting, whether it works in post workout recovery setting, there are multiple ways to test it. And there are certain there are multiple papers that showed either okay, there's positive results. Some papers show that there's no positive results, but there is no detrimental results either. And what you want to do then is to go in dig deep in that pay into that paper and look at the different protocols, the different populations that they use, the different methods that they use, for example, some people some studies, they fast the athletes, some people they the athletes are fully fed Do you know what sort of environment do you want to employ? for your personal use? You know, you have to ask yourself is this papers protocol, suiting my personal preference? Is this reflective of my daily usage of a certain product or my daily lifestyle changes that I want to employ. So I think that's the most important like go, don't let your mind tell you, Okay, I believe X, Y, Z is useful for my health, therefore, I'm just gonna go XYZ good for health, because then then you will find everything under the sun that says XYZ is good for health, you want to say XYZ and say Alzheimer's, don't say good or bad, you literally put the word and that's one trick I use for my during my PhD, is literally do to use two terms. So for example, My PhD was in diabetes and cardiovascular disease, right? So I said diabetes and cardiovascular disease, I did not say diabetes, increased risk of cardiovascular or diabetes causes cardiovascular because that Prime's your question to Google, and that basically frames your frame already. So Google would feed you with information that will reaffirm that, and when you reaffirms that you will, like you said, you turn into opinion, opinions and into identity, and then you run with it. What I want is completely biased. I want the positive and negative. Okay, some people say maybe diabetes cause cardiovascular disease, some people say it just increase the risk. Some people say it has nothing to do, okay, go in there. Why does? Why did they say it has nothing to do with cardiovascular disease, you know, sort of look into a bigger picture. I think, as us, you know, clinicians or scientists or practitioners, it's our obligation to really go into the literature and dig deep, as well as understanding the big picture, and not just want to narrow it down to one mechanism or one pathway. Because metabolism is complicated,
Jade 12:04
incredibly complicated. And I really liked that answer. And one of the things I want to run by you that as a clinician, I feel like is truth. But I want to know, do you feel it's true as a researcher, because you may not, one of the things that I feel is something that I was constantly running into in the clinic is that when I applied one protocol, or one piece of knowledge to one person, I might get an outcome. And if I did the same thing to a different person, I wouldn't get the same outcome. And as I practiced in practice, than I would say, I would start to recognize, well, certain groups seem to do well with certain things. And certain groups don't seem to do well with certain things. But even within those groups, there seem to be variation. And so one of the things that I have, as you know, I would say, one of my laws that I always try to remember is that each person is unique metabolically. And so from my perspective, I would say something along the lines of and I want the expert, you to kind of say, Yeah, Jade, I would agree with that. I don't disagree with that, or I somewhat agree with that. And here's some things to look after. From my perspective, I go, Well, we're each as different on the inside chemically, as we are on the outside physically. And I feel like this presents challenges for the research, it certainly presents challenges for clinicians. And one of the things I've always thought, as I've gone along as they have researched is definitely a tool for averages and very, very important. But it's sometimes doesn't always translate to the individual. And so when you hear me say that, how does that hit you? Is that something you would say? I agree with that, or I don't agree with that, or Jade, you might want to look at it this way. I'm just curious how you see this individual variation that shows up for me clinically, and how it translates for you in the research?
Latt 13:54
Yeah, I mean, personalized medicine, right. I've started, you know, we had to write essays about personalized medicine, even during my master's time in 2008. So during that time, I mean, people already realize this inter individual variability. And it's true, like you've researched cannot possibly capture everything that can be applied across the board. It's impossible, right? Because as a population, we have all these genetic variability is we have this differences in phenotypes genotypes that essentially affect how we live our lives, how we develop as we age, and if we have dysfunction, how we're going to how are we going to treat these different dysfunction? So I 100% agree with you that that's why when you take research, you have to take it with a grain of salt and again, go back to the protocol, what sort of what sort of population are you are you looking at, for example, if these athletes they are if they are doing experiments on 12 athletes, and they're all males, and they're all between 20 and 30. And if you are you know, A postmenopausal woman, then clearly like this will not directly translate to you, you may want to try it trial, you know, just trial and error and see how your body reacts to the protocol. But it does not necessarily is not going to superimpose on to your lifestyle and your age group and your population and demographics. So that's that. And then, as you said, like, our body is very sophisticated chemically, and it's very different and unique, you know, differing from one person to another. And so therefore, whatever approach that you employ has to also be tailored to a certain extent, to the individual or the group, you know, as you said, and I think a very great example is in the brain. And in psychiatry, for example, you can have the exact same symptoms, and given the exact same medications and treatment, and one person could get better, and the other person could have a complete different outcomes. That just shows how, even though with the same symptoms with the same hallmarks of dysfunction, you can still have such variability in the Chemical and Biochemical inside, and therefore reacting differently to the treatment, to the lifestyle change, and to the different small molecules or drugs that you administer.
Jade 16:31
The Yeah, I really liked that question. I'm glad to see that there's agreement there between us, it's kind of cool to see a researcher say, Yeah, we see these individual differences all the time. And, and the way I see it, and I just want to see if you have any other areas individual that we should look at, I see it is like we're unique in our physiology, right, where you our psychology, we're unique in our personal preferences in terms of what we like and don't like. And we're unique in our sort of practical circumstances, you know, some of us live in food deserts, some of us have access to whole foods, things like that is are there any other areas that you would say that we have differences in as well, other than those sort of four buckets that you would say, Oh, we want to look at this as well, you know, we got our physiology, our psychology, our preferences and our practical circumstances? What other areas? Are there perhaps, or does that kind of encapsulated?
Latt 17:20
I think, I think you've basically encapsulated it all in all, because for me, I think, on an individual level, there is, you know, obviously the physical and the mental aspect, which you already said, and then there is a preference, right, and what you prefer to eat what you want your body prefers to now this is the difference, right? What you prefer to eat, may not be what your body prefers to metabolize. So that's also another thing, another process for us to learn about ourselves. So I learned this, you know, personally, that a lot of research, they don't apply to me 100%, it may apply, like 80%, or 90%. But I have to do little tweaks, for example, you know, I see people who, or see studies who feed the athletes multiple times a day, and that increases metabolism. But for me what works best is, or mad, or intermittent fasting, where I eat within a small window of time, and that works really well for me, and it gives me energy still, for my workouts and my activities and, and I still have that cognitive ability and not feel sluggish and fatigued. And then practical, you know, like you said, like, what are your restraints when it comes to practicality, if you have access to a gym, if you have access to a home gym, if you if you literally can move, you know, all day, because you have to be in customer service, you know, stuck in the chair for eight hours. So I think those four areas, you basically highlighted it very, very nicely. I can’t think of anything. Beyond that.
Jade 18:57
You said two things that are really intriguing to me in that sort of discussion. One of the things you said is that if you take you for example, you seem to thrive off of one thing while other athletes sort of thrive off the other end you know, so that's just sort of a repeat what we said but then you said something really interesting was how you got went about you know, sort of deciding what was working for you and you brought up what I would call you know biofeedback sensations, right? It's like is my is my mood is stable is my energy you know, high and in my focus, is my mood good is my hunger under control in my having excess cravings. And it seems like and I oftentimes use this term that in a sense, you know, Dr. Latt is using these biofeedback sensations to decide for himself whether the omad system and for those you don't know that's the one meal a day type of intermittent fasting approach would work for him. So It sounds like what you're saying is like, okay, Jade, like, I'm aware of the research on intermittent fasting and you know, alternate day diets or the Oh, Latt approach, I'm also aware on, you know, you know, many feedings throughout the day. And then I can kind of go into that and say, Well, I do best on this, because in a sense, you're doing almost a clinical evaluation on yourself by looking at how you respond to this. So that's the first thing. And then the other thing, I think it was really interesting that I want to get your take on is that you also talked about the idea that I might, you know, have a personal preference towards what I want to eat. But then when we go down and look at the metabolism and what is going on in our physiology as a result of that personal preference, just because I like something, and I like to do something where I feel, you know, are drawn to that, like, let's say, the keto diet or whatever does not necessarily mean that that diet is doing what we want physiologically. And I think those two points you made are important points. And I just kind of want to get a sense of how you see that, because the way I see it is like, okay, you know, in a sense, we're looking at listening to Dr. Latt, he's essentially saying look, you can be aware of the research, and all the different ways of eating and then you essentially choose one, maybe because you're drawn to it, maybe because someone told you about it, but then you have to decide whether it works for you or not. And it sounds like that's going to be how you feel, which I guess we can learn a little bit about. And it also is going to be about what is happening in your physiology. And we do I guess, have now some tools that we can look inside that. But if you could talk a little bit about how that you think that would work for an individual because you know, we have a lot of people that do keto diets, and I've seen them work wonderfully for some people not so great for others intermittent fasting I've seen were wonderfully for some horrible for others, and I want to kind of see your take on that.
Latt 21:56
Yeah, um, great point. And that's why I you know, in all podcasts that I'm on, I always tell people go out there and trial and error, like, literally just start doing and try it and give time, you know, just doing it for three days for a diet like and then you're like, oh, there's no results or no difference. You have to be realistic, you have to let your body adapt to a different lifestyle, in order to really validate whether or not it works, right. So I always tell people that no one knows your body better than you do, that you are the PhD of your own body. So at the end of the day, whatever information that you get throughout the day, when you do a lifestyle change, when you do a diet change, you will be able to determine if this is good for you. Now, that is assuming that our body feedback, our biology feedback system is functional, healthy, right? There are also times where it's this functional where the rethink, we are getting feedback, but it's actually the wrong feedback. And you know, for example, sugar craving, even though we are not actually craving sugar, and that's when monitoring devices come in handy. So for example, continuous glucose monitors, you'll be able to see, okay, I eat this x food, and it does this to my blood glucose. And then you correlate that back to how you feel. Do you feel bad? Do you feel good? Do you feel sluggish? Do you feel energetic? You can then correlate that so that gives us a check and balance point. Because when we talk about feel and you know, biofeedback, it's very subjective. What is considered good? Well, you know, that's where expertise experts like yourself, Jade come in handy, where people can consult us on okay, this is how I feel. Is this how I am supposed to feel is supposed to be good. I'm feeling you know, lightheaded, kind of like buzzy. You know, when you're on keto diet, they feel like when they have the ketones for the first time, they're like, okay, okay, I feel a bit weird. It's not normal. Is this unhealthy? Am I low blood sugar, am I you know, at the risk of having like hypoglycemia. Whereas other people's know that that's, you know, that's how it should feel. And this is the like, feeling that, that you have that cognitive benefit of ketones, for example. So it's very difficult, and it's a very gray area that nobody has a scale of one to 10 to tell you. This is how you should feel and this is what you know, it is definition wise. So that's why it's very important to check in with your clinicians. Check in with your trainers. Check in with you know, your peers, even if you have friends who are going through the same process, like check in with them and say, hey, you know, I've been doing this, you know, for a while is this how you feel,
Jade 24:58
And let's get back to the show. I love that and one of the ways that I do it and maybe you can either say yeah, that that's a great way to do a jade or maybe add something to this. I oftentimes go from my perspective as a clinician I say look, if your biofeedback sensations are feeling good, I actually have a little acronym I use called SHMEC sleep, hunger, mood, energy and cravings. And so I say, if your SHMEC is in check, that's one subjective biofeedback sort of place where you can say, Okay, this might be working. And then at that point, if we're talking diet and things like that, then I go is your body composition, also obtaining or maintaining an optimal body composition? And then on top of that, and this gets into what you're saying, Dr. Ladd is that this idea of okay, and are your vitals, blood sugars, blood pressures, blood labs, those kinds of things, also moving in optimal directions. And so for me, if we have all three of those things lining up, then I can say, regardless of what I might feel about a vegan or vegetarian diet, or whatever diet this person is doing, or lifestyle, for me, I go perfect. You know, get your biofeedback sensations, the subjective areas are good, we've got the objective body composition is good. And then we've got your blood labs and vitals that seem to also be telling us that this is the right approach. And from my perspective, those three things are a good start. I'm wondering if you could think of any other areas that we might want to look at those kind of have as a clinician, I bucket those things. And that can be tough to do, because there is trial and error in that, as you said, Yeah, but that's how I've always sort of thought about this. And of course, in that in that stuff, SHMEC in check thing, biofeedback sensations. One of the main things with that is also signs and symptoms, if you will, getting headaches and they're getting better, that's going to be a good thing. If you have joint pain and that's getting better. That's going to be a good thing. If you get the disease process is being allayed somehow, and you're having those symptoms, that's potentially going to tell us something.
Latt 31:41
You know, in this past half an hour talking to you, I really love the way you think about things. I really love the way you approach your practice. Because you really look at it at a wholesome level. You don't think of snapshots you don't think of just one direction or one dimension, you literally think about what encompasses life, right? And I'm gonna steal that SHMEC thing and that is such a good so it's sleep, hunger, emotion, mood and craving.
Jade 32:14
Sleep, hunger, mood, energy and cravings
Latt 32:17
sleep, hunger, mood, energy and craving. Okay, got it. That's really crazy.
Jade 32:22
I appreciate I appreciate it expert, like you saying that. From a clinicians point of view. I would I'm excited a researcher finds that interesting. It's sort of a catch all phrase I use for all biofeedback sensations as well. So yes, it's sleep hunger, mood, energy cravings. Yeah, but it's also exercise performance, exercise, recovery, libido, menses, erections, you know, all of these things, signs and symptoms, etc. So I appreciate that. And I want to get into some of your deep expertise now. And this is really just something that I think people will, I want to I've been wanting to talk to an expert about this for some time. Certainly my first book I wrote back in 2010. And I lean pretty heavily in that book on this hypothesis, the carbohydrate insulin hypothesis, I leaned pretty heavy on that, back in 2010. And now in 2020, to 2023, I am pretty convinced that I was completely wrong about that. And it's mostly about calories. Although when I think of quality and quantity and food, I think they're equally important and pretty much inextricable. But I do know that at least in this world of nutrition, and medicine, there's a lot of still debate about this idea that insulin and carbohydrates are the cause of obesity. And this is an insulin carbohydrate hypothesis. Many of my listeners are familiar with this. And I want to get your take on this. And, you know, maybe just give us a brief on what this hypothesis actually has, you know, sort of said, or I can do it, if you prefer. And then I just want to know where you think the research is on this in terms of is insulin, the primary thing that is driving obesity? Is it doing it independent of calories? Are calories what Matters most? How do you, you know, sort of see this issue of, you know, sort of insulin and carbohydrates and where everyone is still essentially talking about this?
Latt 34:19
That that is a very loaded question. Just to put it out there. It's a multifaceted loaded question. So before I go into there, I just want to address a little bit on our previous conversation, because you asked me out of all the three areas, what are the areas you could potentially monitor to see if what you're doing is right, so I would add performance, because if you are working out if you're working on your strength, you're working in an endurance, those are objective metrics that you can easily measure to really see whether or not this lifestyle is good for you. And another thing is, is people are very fixated on bloodwork, some people are super fixated on bloodwork. It's like, oh my god, I'm on keto, my LDL is high. And, and you know, I got to change this and that, make sure you understand that blood work is essentially a snapshot of your metabolism is by no means I'm describing your entire flux of metabolism. So you know, know that what you did, right? Before you take the blood, you know, is asleep, okay? And everything, like it really affects that snapshot. So, you know, talk to your physicians, talk to experts that can really decipher and interpret your blood results for you. So that's that. And then back to your question on insulin and carb, you know, are they the culprit here. So, what I always tell people is that because metabolism is not about a switching on or off thing is not a yes or no thing, it is a Goldilocks zone, optimal amount of thing. So we need insulin, absolutely, we need insulin to control blood glucose. But if we have access of glucose, and glucose elevation for the entire day, then you get an elevation of insulin for the entire day. And that's when a problem occurs, because we're not made to do that we're not meant to have high blood glucose throughout the day and high blood insulin throughout the day, you know, back in prehistoric human beings, you know, you probably don't even have access to that much carbs. And people are moving around hunting, and they have, you know, they live and proteins and fats, and they possibly fasting before they go for the next hunt as well, because, you know, they only hunt for what they what they need to eat, because they have no storage system, right. So in that sense, like, our modern nutrition, quote, unquote, modern nutrition is exposing us to physiological changes, that was not there in the past before evolution, sort of point of view. And because of that, it's causing our metabolic pathways to go in and dysfunctional direction. So I would say the constant elevation of glucose and insulin are causing potentially inflammation. And of course, even if it's not blood glucose, if you have moderate glucose and high fat diet, that itself is signifies, you know, calorie excess surplus of calories. So where does that surplus go to it goes into storage, it accumulates as fat. So that increase in adipose tissue in research has been shown to increase adipokines and inflammation markers, and that also perpetuate the insulin resistance within your other organs, especially in muscles. So when that happens, you know, you are telling the body, hey, there is a lot of glucose muscles was not getting in glucose, because it's insulin resistance, because insulin sends the signal says, pull into glucose, metabolize it create energy for movement, but your muscles are saying that, Oh, the doors are locked, you know, I can't take in glucose. So it's sending the signal to the pancreas, which secretes insulin says we might need more glucose, sorry, we might need more insulin, because these glucose are still circulating in the blood. So they pump in more insulin. And then that cycle of the vicious cycle continues until to a point where your pancreatic beta cells start failing. And that's when you you get you know, diabetes, and you have to inject insulin and all your muscles are just haywire because it doesn't know what substrates to use, it doesn't know what substrate to pull in. And because of that, like it causes the whole myriad of metabolic dysfunction. You know, obesity, increasing Heart, heart disease, increase in risk for diabetes, high cholesterol, high blood pressure, all of that are all linked together. It's not just one thing, it's not just okay, carbs is bad for you. So if you avoid carbs, then everything will be solved. Like you still have to look at your calories, you still have to look at your physical activity, you have to look at your sleep, you know, people have a lot of studies have already. So sort of attributed increased risk of cardiovascular disease and obesity with lack of sleep, or the too much sleep. You know, like I said, it's, it's our human body likes to work in an optimal zone. That's why when you look at enzymes, and you look at hormones, even when they do it in vitro, meaning that they do it in cell cultures, they isolate them so that you can easily you know, monitor the changes. You always have to provide the most optimal pH the most optimal temperature In which they will behave optimally, anything above or below that, it will cause a dysfunction, whether it doesn't work efficiently, or it just work in a way that tries to compensate for that lack of optimism, and that may cause damage to the body.
Jade 40:22
That's perfect. So let me just repeat what I think you said for you know, and just maybe add a couple things and see if I'm getting this right. So it sounds like, what you're essentially saying is you're saying, okay, Jade, you can overeat carbohydrates, and you can get this insulin, the excess insulin production, that is not a good thing, not necessarily because insulin is high or low, it's that we don't want either of those situations, we kind of want insulin in this Goldilocks zone. A couple other things I'll add, and then you can kind of tell me if I get this right. And well, my understanding is you can also be insulin sensitive or insulin resistant in certain tissues. So if you're insulin resistant in the liver, for example, that has a particular impact, you can be insulin sensitive or insulin resistant in the muscle that has an impact. Insulin is a hunger hormone, either directly through either because directly it signals of satiety in the brain and or through its impact on leptin. So there's lots of going on with insulin, so we had insulin super low, then we wouldn't be able to get food into the body to begin with, that might be hungry all the time. But when we have insulin super high, we also run into these other problems, then you essentially said, well, Jade, also, if you started overeating fat, nothing but fat, but you were increasing calories and started to produce excess adipose tissue, that adipose tissue would start to send certain signals some of those inflammatory in nature, which could then cause insulin resistance as a result of that those inflammatory signals. And then one other thing I'll add here is the impact of stress, which you alluded to with sleep, stress. And cortisol also can have a negative impact on insulin sensitivity. So in a sense, we are having multiple factors that can impact insulin. But the question that I just want to make sure that, you know, the listeners don't miss is if, let's say your insulin resistant, and you have a lot of insulin in your system. And you're not going to think about cutting carbohydrates at all, but you don't have excess calories, you start to have a calorie deficit. With high insulin, will you still be able to lose weight if you're in a calorie deficit with high insulin? Or does that high insulin keep you from losing weight? Or does it impact for example, the percent of weight you might lose?
Latt 42:47
I think I think it would definitely impact that effect. But I think it goes back to what we talked about earlier, the inter individual variability, I think it depends on the person, right. And it depends on what sort of training program they're going through as well. Right? If they are doing some form of resistance training, that could potentially increase insulin sensitivity and muscles, then potentially that could lower that insulin secretion and insulin elevation. And over time, with the calorie deficit with the right workout increasing insulin sensitivity, there may actually fix it. And we have seen this many times. For example, Virta health have done amazing work in reversing diabetes using ketogenic diet, and also lifestyle changes. So it's not impossible to achieve that. But you just need to know your body well enough to know what works for you, and what works for you at this time. Because four months later, you might have to employ a different strategy because now your insulin sensitivity level is different, your weight is different, your appetite is different, your calorie intake is different. And because your weight is different, you need to adjust your calories accordingly as well. So there's no one size fits all solution. It's an ongoing process as a life journey, the way I see it, and that's why I enjoy it. And that's why I love it because you don't know what's to come next. You know, you trying all these different things. And recently I've been doing my own experiment on myself on male allergy because I cut out dairy for a bit and when I reintroduced it I realized I had, you know, some minor hives and I was like, as weird is it melt? So I was like trying to do an elimination process and try and figure out is it just milk or is it cheese is everything dairy, and it turns out, cheese doesn't have a lot of problem with it. My protein powder, which is a combination of whey casein, and milk isolate, didn't give me any problem, but drinking milk does. So it's super interesting. And you know, now I'm like trying to troubleshoot this. How can I I fix it joy, introduce milk little by little again, or do I avoid it altogether? I'm still for green bow, and I've been trying to look around on the science, there's not much there's a lot more on infants, infant milk allergy, but not adults. So I've been talking to different individuals, different contacts that I have, you know, clinicians and people who have been dealing with allergy or their lives. So if you have any opinion, please, please. I mean, I'm all ears.
Jade 45:24
Yeah, well, it's interesting. This is this is a question that comes up for me a lot where people bring up food allergies and food sensitivities. And you, you kind of alluded to this typically, that's a food sensitivity reaction. The other thing that's interesting is that the testing that you do for food sensitivities is really not regarded by most of us who are up on this in the functional medicine world as reliable. And so the only real way to do this is exactly what Dr. Mansor did, where he's basically taking the food, eliminating it for time adding it back in and then looking at these biofeedback sensations. This is exactly the way that I would do this in clinic, because I don't regard and I've run 1000s of those food sensitivity tests at one point, I don't regard them as accurate in determining what you're actually sensitive to. And I don't know if you have anything to say on that. But, you know, I think we've lost, there used to be, you know, 10 years back, I was thinking, Oh, IgG reactions versus IGE reactions. And now it looks like you know, these IgG reactions really aren't telling us what we thought it was, they were telling us about the immune function. And so at this point, without knowing more, this sort of Allergy Elimination or food sensitivity, elimination diet, and adding back in is also the way that I would do this as well. So that's exactly the the process that I would use. And I do think it has a lot to do with and this actually comes back into sort of your expertise as well. I do think it has a lot to do with for example, milk, especially high fat milk is also a pretty significant source of estrogen and progesterone, bovine sex steroid. So that might be playing a role here. Fat is really interesting, because fat is something that lipopolysaccharide LPs, you know, that little, you know, endotoxin that sits around in our gut kin, that LPS can jump on the fat from milk and perhaps be driven into the system and cause inflammatory reactions. And so when I'm looking at certain foods that might be causing reactions, I'm looking at those kinds of things. I'm saying what could this be doing to trigger inflammatory reactions that aren't just simply about, you know, the IGE or IGE mediated reactions? So I look at these inflammatory mechanisms. And actually, one thing I'll, I'll tell you and see, I'll give you my theory on why it happens, because you're the expert in in keto diets, one of the things that I noticed when I used to put people on keto diets, certain types, these would typically be the people who were fairly obese diabetics, you know, obviously, they tend to respond very well to keto diets. But one of the things I saw on a significant subset of these individuals is the keto diet would essentially cause you know, this keto flu, and by the Keto flu, when I talk about it feels like the flu, they had aches and pains, almost like they were waking up, you know, after a hard set workout or had the flu. And one of the things that I thought is that most of these people were eating high carbohydrate diets, obviously increasing those gram negative bacteria, and the ones containing the LPS. And all of a sudden, you dump a lot of fat into that system, that LPS can get, you know, sort of put into the body and cause this sort of mild endotoxemia. This is the way that I've always seen it now, after a little bit of time, that goes away, and they tend to get results. But for some it was a pretty severe reaction. And that's, I'm not sure that that's the mechanism that's going on. But it's certainly something I've seen, and I wonder if that has something to do with it. And if you all at home, if we just got a little too technical for you. Let me just briefly tell them Dr. Messer, what LPS is just, it's sort of like these little bacteria live in your gut. And when they die, it's almost like they're wearing these fur coats. And when they die, they shed these fur coats and those fur coats then can get brought into our systems in cause inflammatory reactions. We call this LPS or endotoxin. It used to be thought that this LPS could not pass through the system. And if it did, you'd get septicemia. But now we know trace amounts can and they have reaction. So my question to you is, do you think this is something that's going on? Do you know much about this? Do you think keto diets predisposed to this in the short run and, you know, maybe help in the long run? Is there any hints you can give us about this? Because it's always been interesting for me as a clinician to see this.
Latt 49:41
Yeah, I think I think that's definitely that definitely could be one of the mechanism that drives it. Another well-known mechanism is that when you switch on keto diet, you are essentially shedding all your glycogen stores, because you are cutting out carbs, you know, very restricting restrictive amount of carbs every day, therefore your glycogen stores will then diminish. But glycogen stores are known to store water. And with water, we also store a lot of our salts. So when you lose that large amount of water and glycogen, you're losing a lot of different micronutrients, like, you know, sodium, potassium, magnesium, calcium, and those salts. Those ions are also very important for neurotransmitters for all sorts of Transportations of molecules within cells. So when that happens, you know, the body is trying to compensate, or the body is trying to send signals to you that, hey, something abnormal is happening right now something dysfunctional is happening, do something about it, right, or the body is doing something about it. And inflammation is a response, when there is something abnormal happening in the body, right, whether it's a foreign invasion virus, bacteria, or inside, where it's too high amount of fat, you know, like we talked about too high amount of insulin for too long, too high amount of glucose for too long, that sort of thing. So, you know, it should be a combination of factors that cause that keto flu, but also remember, every time we switch to a new diet, we switch to a new lifestyle, there is always a big change in the body that the body needs time to adapt. And if, you know, inflammation is one way of the body to adapt. And there are some research that shows the change in micro biome in your gut as well. And that itself could also cause inflammation in the short term, because of the stopover in microbiome as well. And, and that's why I always tell people to be mindful of labeling certain thing or demonizing the same thing. It's one thing when it comes to virus or bacteria, we can say okay, COVID is bad, you know, we know that right? But when we talk about Oh, am tau is bad, insulin is bad, leptin is bad, ghrelin is bad, or like, or something is good. It's not necessarily that you have to look at it in a much more wholesome picture where, okay, elevated insulin for a long time as bad, not necessarily insulin on its own is the dysfunctional level of insulin, because all these hormones exist in our body for a reason, right? We, we evolve to a point where we need all these different hormones every, each single one of them to function properly in order to be healthy, and in order for us to function properly. So when there is something that goes out of whack, that's when things go wrong. And, you know, traditionally in medicine, we figure out what that is what is going wrong, and then we pinpoint that. And then we straightaway say, you know, oh, that's a bad thing. Not necessarily true. So I think if there's any takeaway from this, like, go back and look at different biomarkers, different hormones differently, you know, you want all of them to function properly, but you don't want to eliminate them or increase them unnecessarily.
Jade 53:21
Yeah, one of the things that I've seen in this space is what I would call mechanism chasers, there are people who learn a biochemical mechanism, they don't know many other biochemical mechanisms. And so they treat it almost like a bow and arrow hitting a target and they go, everything must fit this biochemical mechanism. But it's not a bow and arrow hitting a target. It's more like a spider's web or a symphony. And all these things are working together, I'll have to say, you know, hormones in particular are sort of like people, they behave differently depending on who they're socializing with. So for example, in, in exercise, you have high cortisol. And that's not a problem, you want high cortisol levels during exercise, it just tends to come along with also high amounts of human growth hormone and testosterone and insulin sensitivity versus when you're sitting at home sitting on the couch. Now, cortisol and insulin are primarily, you know, having, you know, dinner together, socializing together, and that creates a different sort of outcome. So we're running up on time, we got about 15 minutes, I'm loving this conversation. Let me ask you about something that I noticed when I was reading a little bit about you, you talk about the idea that and I love this because when we talk about metabolism, and you have people who are experts in metabolism, most people want to talk about metabolism as fast or slow. They want to talk about stimulating metabolism or boosting metabolism. And one of the things that you talk about is this idea of metabolic flexibility. It's something I talk about as well, where I oftentimes say we don't necessarily want a fast metabolism. We want a flexible, responsive adaptive metabolism, which is correct really what metabolism is when we think about it as a responding, you know, sensing and responding apparatus and so we You want it to be able to sense appropriately and respond appropriately. So one of the things I want to ask you about in this realm is, if you could talk a little bit about this idea of, you know, how true is it to talk about metabolism, or fast as fast or slow? And if that is the case, how come we can see certain things like cold plunges and exercise certain these things can certainly speed up metabolism and even increase fat burning in the long run. But then when we look at actually controlled trials of these things, over weeks, they don't necessarily seem to deliver us weight loss results. And a lot of people, you know, sort of are confused by this. I wonder if you can just set me straight and set the listeners straight a little bit on this idea of how should we be looking at metabolism? Should we be trying to speed it up? Slow it down? Make it more flexible? How do you know, sort of have this conversation in your head based on the research you've done?
Latt 55:55
Yeah. So it's funny, you mentioned that because we have been in conferences before where we, you know, have samples of exogenous ketones of ketone IQ. And people would ask me, it's like, so as a research lead, do you think this ketone IQ can make my metabolism faster? And I'm like, oh, boy, where do I start with that? Very question, right? So when people talk about fast and slow metabolism, essentially, they just want to know, will I be able to burn calories, fast, and a lot of calories, given the amount of food and given the lifestyle that I have? I think that's the general understanding, right. But most importantly, a lot of people associate that with just exercise, like you said, if you exercise two hours a day, right, there's still 22 hours in the day that you're not exercising, those are the hours that actually Matter even more, because that that contributes to your basal metabolic rates, that the non exercise and energy expenditures, increasing those activities like standing up walking, walking around, you know, between breaks of your work, and those are the things that actually increase, quote, unquote, increasing metabolism, but it's actually increasing your energy expenditure. When you increase your energy expenditure, you put yourself in a calorie deficit, so that is matched with your calories, right. So even if you increase your energy expenditure, but if you're eating a lot of calories, that still means calorie surplus. And, and on top of that, you know, we can also talk about what kind of calories, you know, certain foods will then induce a certain response of hormones, right? High carbs, food, obviously induce high insulin? And how would that make you make you feel right? If you feel sluggish, if you feel fatigued, then you feel less motivated to go work out? Right? You also have it's not just calories in calories out? Yes, fundamentally, is fundamentally it is calorie and calorie out. When you have calorie surplus, you will, you know, tend to put on more fat and storage, when you have calorie deficit, you tend to burn more and lose weight. But ultimately, also, what kind of food you eat, also affect your microbiome, affects your mood, affect your sleep, and affect your hormones, your stress hormones and all that. And that would also affect the activity you do. And then it goes around, right? Yeah, activity, and then and then your food. So in terms of metabolic flexibility, this is exactly why we pitch about metabolic flexibility, because you want your body to react to a stimulus that you put your body through, at that time in the most optimal manner. Which means if you're doing X, for example, if you're doing endurance exercise, you want your body to tap into that, that that glycogen stores that you know, fat source because you're going on a constant pace fat, can you no continuously give you that that energy that you need. But when you go into like high intensity workouts, when you go into resistance training, you want your body to swap over to glucose, because nothing beats Glycolysis in providing oxygen independent ATP, which has energy to fuel that sort of high intensity workouts. So when your body is that good at swapping, you know, to the optimal fuel one you perform optimally to your body is able to then you know, use whatever is necessary and store only whatever that's necessary. So that signal that your muscle is sending to your brain is sending to your storage is sending to your liver. It's all in sync so that you are in the optimal zone.
Jade 59:46
And now back to the show. I love that answer. And here's another question for you about that. So would you say and especially I want to talk a little bit about these exogenous ketones here in just a second. But would you say that female and male metabolism is any different in this regard? For example, how is estrogen you know, and progesterone in the female menstrual cycle? I know this can be a tricky thing to study. Because when you're looking at women, you would have to match menstrual cycles in order to you know, still really get this and or understand where they are follicular phase versus luteal phase. But I'm wondering from your perspective, how you see any differences, just generally in metabolism, from men to women, I oftentimes talk about the idea that, you know, men and women the female metabolism is a little bit more, I don't know how to say it may be refined and sensitively are, after all the gender of childbearing and estrogen and progesterone, these fluctuations do kind of put them in different metabolic states one half of the month, to the other half of the month, and certainly go through different lifestyle stages, you know, based on these hormones, I'm wondering if you have any, you know, sort of insight on this from the research perspective, and how keto diets might be impacting women versus men differently. What the menstrual cycle, you know, how it impacted any of those, those things? I'm just curious.
Latt 1:03:41
I think a lot, um, a lot more studies these days that came out that showed the differences between genders, between males and females, and I think I listened to podcasts before and, and they were saying like, you know, females are not tiny males, you know, just because. And they do react differently to different lifestyle interventions, different diet interventions. So one thing that at least in animal work that I've done during my PhD, the whole reason of selecting male only rats, it's because of that is because of the fluctuation of hormones during menstrual cycles. We don't want to deal with that, especially when it comes to diabetes, because during that hormonal fluctuation, you see a fluctuation of blood glucose and home and other hormones and insulin as well. So we want to induce a type two diabetic rat, we want something that is stable, so we know for a fact that it is the high fat diet and is the drug that makes the rat diabetic and not working synergistically in some manner with the hormones. So yes, to that point. We need more gender specific studies that look at different stages of menstrual cycle and how that affects females. Because we have a lot of male driven and male focused studies already. So we know what works within the male population. But now we need more sort of female population and see how that impacts them. And you know, is that, for example, there is a study on ketogenic diet that affects postmenopausal women differently to pre-menopausal women. So even that within those two demographics is already different. So let alone you know, comparing me men and women.
Jade 1:05:33
one of the things I'm not sure, you know, but one of the things about my work is that I mostly worked with women, and mostly saw these differences very early on in my career, and I've gotten a lot of a lot of love and a lot of hate from, you know, making that distinction over 10 years ago saying, Look, we really need to treat women differently. I mean, obviously, estrogen is highly insulin sensitized. So if estrogen is around, that's going to play a role. And when it goes away at menses that's gonna play or, you know, menopause, post menopause, that's gonna play a role. And I think, you know, this isn't completely sort of worked out yet. But it's interesting. And one thing I didn't know is I did not know that about the, the laboratory rat, is that kind of standard across the board when you're doing diabetes stuff, where you're just like, we're gonna male rats only to take these estrogen and progesterone sort of things out of the out of the picture.
Latt 1:06:23
Generally, yes, most importantly, yes. So because if you're already dealing with animal animals, models, the whole reason of dealing with animal models, because it's more convenient compared to clinical trials, obviously, you don't have to go through IRB, you don't have to go through ethics committee and all that. But if you're already choosing that route, why not, you know, eliminate all the other variables to mean when it comes to science, right. At the end of the day, we are essentially doing an elimination process when we investigate certain things. We're doing elimination prototype process, we're trying to eliminate all the variables that may affect our results. And then we introduce variables that we think may affect the results so that we can for sure, say that okay, x y Zed is what's causing a certain disease, or x, y Zed is what's improving certain conditions. Yeah, so that's a great, so the more the more variables you can do, the more variables you can eliminate.
Jade 1:07:23
We'll bet 100% Well, let's take the last five minutes or so and talk a little bit about I'm curious about the idea of exogenous ketones, I've heard all that. So just for the listeners that understands. So you can you know, go on a particular diet and entice your body, usually a very low carb diet, you know, carbohydrates, usually less than 10%, fiber said he talking maybe 30 grams to 50 grams of total carbohydrate, and you can stimulate, you also have to have your protein relatively moderate, because you can have gluconeogenic amino acids, but typically, we can do this through diet, well, we can turn on ketone production, we can have many beneficial things we know the science has been in the last 10 years has just been huge in this area. One of the things you also can do is you can take ketones, this is from an outside source, exogenous. So one of the things that the lab studies is he studies exogenous ketones and how they impact our body. So what is the benefit here? Because you know, I one of the things I know about ketones is ketones can be muscle sparing ketones can be hunger suppressing. ketones can have lots and lots of different, far ranging impacts on metabolism, mainly, very good impacts, since we don't spend a whole lot of time in ketosis the way we did as historical man. Are we seeing the same thing when we take these exogenous sources should somebody who is not an athlete, just a regular person who wants to be healthy, consider taking exogenous ketones and how do they work? And why might they be beneficial?
Latt 1:09:00
Yeah. So the answer is yes. And yes, but and this is not just me being employed by HVMN. It's literally what the research has shown. Right? So research showing brain network stability, for example, in aging adults, they put people on a ketogenic diet for a week and they give them exogenous ketone for one dose, both the group show improved brain network stability within the functional MRI, compared to placebo. So in that sense you are getting because ketones are ketones or ketones, is the same molecule is the same thing that is getting metabolized and sending signals to your body in order to get the benefits. Now the difference is yes, exogenous ketones can only keep you in ketosis for X number of hours before you have to top up again. So when you say you know what type of people may be beneficial in taking this anyone really even if you're on a ketogenic diet, because a lot of people a lot of our customers was like it You know, I'm taking it, I'm doing a ketogenic diet to lose weight. I'm doing ketogenic diet to do to get cognitive benefits. So why should I take exogenous ketones when I can make my own? And the answer is you don't have to, if you're already in ketosis, if you're already making your own ketones, go for it, like, like, enjoy that lifestyle and reap all the benefits. But if you feel like you can benefit from increasing that ketone, pumping that ketone levels, which is blood BHB, beta hydroxybutyrate, a little bit more than use it as a supplement. So what I always tell people is that first of all, you have to dial in on your lifestyle, your nutrition, your physical activity, your sleep, you know, and then you take in supplements to further enrich that. So this is the exogenous ketone that I'm talking about, I use exponential exogenous ketones to enrich my lifestyle that I already like, you know, work so hard to get in place first. And that is also why, you know, some people prefer to take it, if they cannot do a ketogenic diet, for example, they love carbs too much. Or, for example, they have family, and if they do it themselves, they have to cook for their family, and they can't, and then it's just less flexible. exogenous ketones provide that flexibility. For our $6 million contract with the Department of Defense, for example, with the military, you can't make the military going ketogenic diet, all of them, you know, just to get that benefit, that cognitive benefit, right. So this is the best solution for them, because you get that boost for few hours, like when you need it, you know, on demand. And you get both the physical and cognitive benefits. And we saw an improvement in adaptation to hypoxia on top of that. So that is huge when it comes to operations in high altitude, for example. And if you can make faster reactions, you can make better decisions. And you can, you know, really be on point and focus just by drinking a shot of exogenous ketones, versus having to put them on a ketogenic diet for a few weeks before they get into ketosis. That's, that's where the value comes in. Yeah. All right. So you want and also for people who haven't done keto diet, thinking about it, and want to sort of feel how it would feel like to be in ketosis, or to have ketones in your body have a shot, you know, have that feel like one of my friend literally texted me, I sent a bottle to them. Last week in New York, and he just texted me this morning, he was like, Yeah, I feel focused, but in a calm way. And that's a common feel. Because when people say focus and alert, they think of coffee, they think of stimulant. And people expect like jittery feeling people expect, like, I want to go, I want to, you know, my heart is pumping. But this is more of a calming feel, but you can still focus, and I usually drink it before our podcast, and I did drink a shot right before this. And it helps wire my brain to my mouth so that it's very coherent. My thoughts and what's coming out. It's coherent. You know, and consistent.
Jade 1:13:17
Yeah. Yeah, I love it. Let me ask a couple of questions related to that, you know, typically, when we're in ketosis, we should have, you know, sort of low blood sugars and high ketones. So glucose, low ketones high as Matter of fact, one of the things we do clinically is we look to see if someone is having problems we go is glucose high and ketones are not a good thing to have what we want as ketones go up, we want them coast to build down and you can even see that very low glucose values. With high ketones. Some people are like, am I going to be hypoglycemic i values at 40 and 50 blood sugar levels, but the ketones are keeping them functioning. So when for these to work? Are they still working if the glucose is high? So for example, if I eat, you know, wake up and have, you know, some breakfast cereal and then take my shot of ketones? Am I still getting some of the benefits? Or are they sort of wiped out?
Latt 1:14:11
That's a very interesting question. Now, as you said, physiologically, it's impossible to have both high glucose and high ketone without exogenous ketone, right? So that's, that's why a lot of people are like concerned. So is this you know, this is an abnormal physiological state is this okay? In fact, it is more than okay because we have seen it in performance athletes. way they use a dual fuel, where they have a dual fuel system and they would have carbs and exogenous ketones, and that has glycogen sparing effect. So for endurance athletes, they found themselves being able to push themselves further, because they have that dual fuel. And what we have seen in terms of organ specific, we look at the brain and the heart, even with the presence of glucose, fat, and ketones. Um, the fat and the sorry, the brain and the heart, they take in ketones proportional to the availability of ketones. So for those of you listeners, certain, every organ, we need certain transporters to transport these molecules into the cells. So we need glucose transporters, glutes, if you have heard of glute one, glute four, those are, you know, very prevalent in the heart. So you need to transport the glucose via glutes, you need to transport fat fatty acids using fat trans fatty acid transporters, CD 36 is one of them. And ketones also need transporters, which they share the same transporter as lactate, which is monocarboxylate transporter. What we have seen in research is that at some point, the transporters get saturated for fat and glucose. So they will go up go up, you know, and even at a very high level of glucose, it will still plateau out because the transporters are saturated. What we have seen in ketones, for example, surprisingly, is that it's keeps going up maybe in the research in the protocol, they haven't got high enough glucose to plateau. But even when ketones are present, the heart is taking in ketones without affecting the other uptake of the other substrates. So that is very interesting. So essentially, providing your important organs like you know, brain and heart, the extra fuel that you need for whatever activity that you're doing. So I would say like us, I think exogenous ketone can benefit everyone, but use it in the right use cases.
Jade 1:16:44
Yeah, that's, that's fascinating to me. So let's go through a couple of those you use cases, and I'll let you go because I want to be aware of your time, but you're just it's just really nice to have you on here. So one of the things I would think of ketones certainly have hunger suppressant activity. So are these exogenous ketones able to help us with things like hunger and cravings? And have you seen that?
Latt 1:17:05
Yeah, so I personally use it myself. Like I said, I do Omada, which is one meal a day. And usually I'll have ketones the night before. So technically one meal a day, but I'm still consuming calories from ketones during the night. But after that, it keeps me you know, perfectly satiated until the next day lunch. Yeah, so you know, use it to prolong their fast.
Jade 1:17:32
Yeah, so it doesn't say not only prolong your fast, but uh, you know, one of the things that you know, that we you look at in the research, as you can see that even small amounts of calories up to 500 calories in a day, you still get some of those fasting benefits metabolically. So I imagine, if you were someone who struggled with fasting, and you took these exogenous ketones as sort of, you know, like a fasting beverage, you're gonna get very little calories, but you're gonna get some of this boost. And I imagine it would be effective here. Is there any other things that, you know, you find interesting that these things do that not a lot of people are talking about?
Latt 1:18:07
Um, yeah, I mean, so the common use cases are, you know, fasting appetite suppression performance, where people take it before workout, they'll take a want to dose with carbs, not replacing the carbs or any pre workout you have. I sometimes take it for recovery as well. So it doubles up as a recovery and hunger suppressant because studies have shown that taken with ketones, I mean, sorry, taken exogenous ketones taken with carbohydrate and protein, increases mTOR activation, protein synthesis, after workout. So that definitely helped with recovery as well. Most people use it for just the cognitive benefit, just the focus in the day to have it one in the morning. If, especially if they're fasting, they really keeps their, you know, mine in tip top condition, and then they can continue the fastest. Well, and that's very interesting, what you just pointed out, like 500 calories because, you know, fast mimicking diet. It's around like 500 500 calories. And, you know, at first I thought, you know, that's just a calorie restriction and not really fast, per se. So I think there is a certain leeway over threshold of what is considered fasting to your body, and what is considered calorie restriction.
Jade 1:19:35
and I'm sure what that what those, you know, I wonder how much autophagy which I know is somewhat controversial anyway, you know, we know it happens in rats. We don't know how much it's happening in humans. But there are other things that, you know, that that that, you know, maybe having no calories at all might help you get into autophagy faster or something like that. But
Latt 1:19:53
yeah, and that's why I usually tell people if they fast in order to lose weight or in order to eat less than Yes, exogenous ketones can definitely help. But if they're fasting to achieve autophagy, do keep in mind that ketone IQ, for example, has calories. It has 70 calories per dose. But if you think about it, though, 70 calories you can burn off in like, you know, especially if you're exercising on top of, of being fasting long time to get the autophagy. It will just help you feel less hunger hungry.
Jade 1:20:27
I've been becoming more and more interested. I've tried exogenous ketones in the past, I had really good effects with them. I don't know why I stopped.
Latt 1:20:36
have you got samples from ketones?
Jade 1:20:38
I haven't had samples from you all. Yeah, no, I have not. But I certainly I certainly, you know, having this conversation with you certainly makes me go Oh, yeah. You know, those were used to be really, really useful for me in many ways. And that's when I was fasting a lot. Actually, I was used right and same way that you're using them, but I'll tell you what, not their Latt man, sir. Thank you so much for being here. I mean, you're just a brilliant guy. incredibly generous. I'm so grateful for your expertise. Where do people find you? How can they get, you know more involved with your work and keep up with you.
Latt 1:21:11
And you can go to our website at www.HVMN.com and HVMN on all handles on all social media. And you can find me personally last month, so LATT MANSOR on Twitter and Instagram, so and I do also do weekly IGS. Monday morning and Thursday mornings with our affiliates. We're experts in gut health and metabolism, just to have a more informal session for half an hour and engage with our customers and listeners, just you know, whatever questions they have, come on and just ask.
Jade 1:21:46
That's great. I'm gonna I'm definitely gonna follow you my friend. I appreciate you so much. Thank you for being here and hanging out on the show with us.
Latt 1:21:53
Thank you so much for having me Dr. Jade
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.